Patient Education
Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein.
Topic Contents
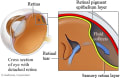
Pneumatic Retinopexy for Retinal Detachment
Surgery Overview
Pneumatic retinopexy is a surgery to repair certain types of retinal detachments. It is usually an outpatient procedure, which means you don't need to stay in the hospital.
Before surgery, your eye is numbed with local anesthesia. Then the eye doctor (ophthalmologist) injects a gas bubble into the middle of the eye. Your head is positioned so that the bubble floats to the detached area and presses against the detachment. The eye doctor then seals the tear in the retina using a freezing probe or laser beam.
The bubble helps to flatten the retina until a seal forms between the retina and the wall of the eye. This takes about 1 to 3 weeks. The eye slowly absorbs the gas bubble.
What To Expect
It takes about 3 weeks to recover from this surgery. The hardest part of the recovery is keeping the gas bubble in the right place.
- You must keep your head in a certain position for most of the day and night for about 1 to 3 weeks after the surgery.
- You cannot lie on your back. If you do, the bubble will move to the front of the eye and press against the lens instead of the retina.
- You must avoid air travel until your eye has healed. A change in altitude could cause the gas bubble to expand. This would increase the pressure inside the eye.
Why It Is Done
Pneumatic retinopexy is done for certain types of retinal detachments. It can be useful when:
- A single break or tear caused the detachment.
- Multiple breaks are small and close to each other.
- The break is in the upper part of the retina. You have to hold your head so that the break and the bubble are at the highest point. This is not practical if the break is on the bottom of the eyeball. You would have to keep your head upside down.
How Well It Works
You are more likely to have good vision after surgery if the macula was still attached before surgery. Good vision is less likely if the detachment affected the macula.
Risks
The most common problems after this surgery include:
- Scarring on the retina. This often causes the retina to detach again. Scarring is the most common reason that surgery fails.
- New breaks or tears forming.
- The need for more surgery to reattach the retina.
- Fluid that stays under the retina or is absorbed very slowly.
- Small gas bubbles getting trapped under the retina.
Less common problems include:
- The detachment spreading into the macula. This affects central vision.
- Higher pressure in the eye. This can lead to glaucoma.
- Cataracts.
Credits
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024-2025 Ignite Healthwise, LLC.